ORCID: 0000-0001-7090-2091
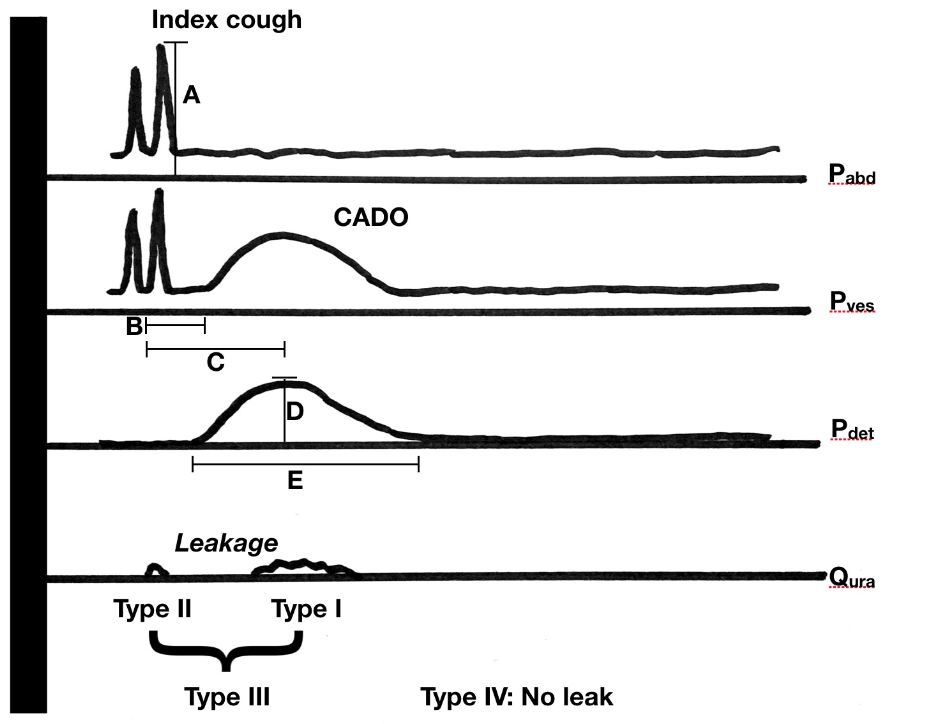
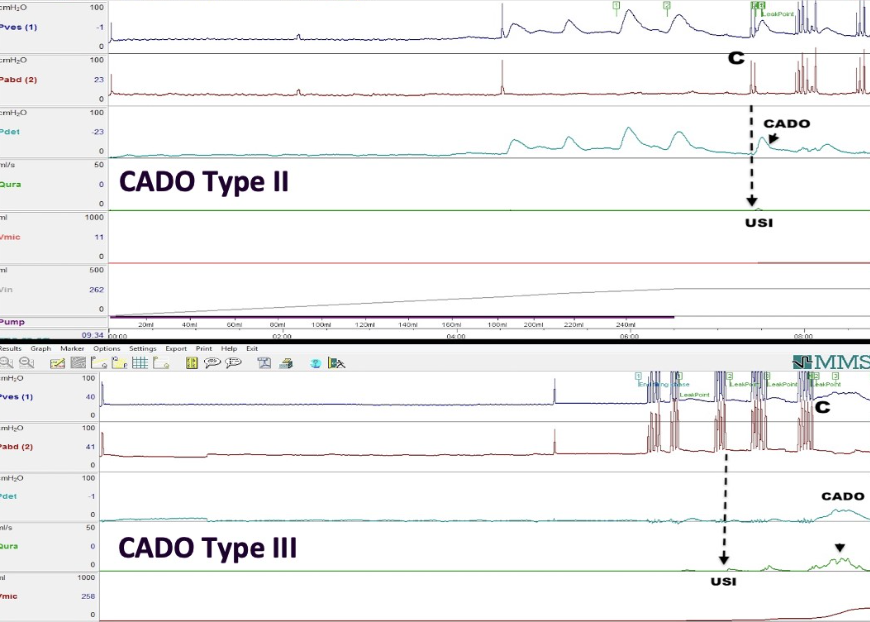
It has long been recognized that a phasic bladder contraction can be provoked by cough. This phenomenon can cause or aggravate urinary incontinence and is a confounder of the clinical stress test used for diagnosing stress urinary incontinence in women. There has been a lack of clarity with regard to what this entity represents and the best way for its management. Several different terms have been used for this condition causing further difficulty in the interpretation of literature. However, the International Continence Society now recommends use of the term cough-associated detrusor overactivity (CADO) to describe the condition.1 These patients have usually been managed as a form of urgency incontinence or sometimes, by stress incontinence surgery. However, as we have published, CADO can take four different forms, potentially having differing implications for management (Figure 1).2 Briefly, CADO can be classified based on whether the accompanying leak occurs with the phasic contraction (type I), the cough (type II), with both (type III), or with neither (type IV). CADO was noted in 2.2% of women with urinary incontinence presenting for urodynamics. Type I was the commonest while type III was the most bothersome. Clearly, while stress incontinence surgery might be indicated in the carefully selected patient with type II or type III CADO, it is unlikely to ever be appropriate in type I. It is possible that a combined approach of using botulinum toxin at the time of stress incontinence surgery might be useful for those with type II or III. Unfortunately, a study reporting on such combined therapy missed the opportunity to classify CADO.3
Currently, there is an imprecision in the diagnosis of CADO. Use of the CADO classification provides a precise label that can convey, unequivocally, the urodynamic finding and nature of underlying etiology behind incontinence. Wider usage of the classification is likely to result in higher quality evidence that, in time, could result in more precise recommendations.
References
1. Rosier PF, Schaefer W, Lose G, et al. International Continence Society good urodynamic practices and terms 2016: urodynamics, uroflowmetry, cystometry, and pressure-flow study. Neurourol Urodyn. 2017; 36: 1243–1260
2. Sinha S, Lakhani D, Singh VP. Cough-associated detrusor overactivity in women with urinary incontinence. Neurourol Urodyn. 2019;38: 920-926.
3. Hajebrahimi S, Shamsi-sisi H, Jahantabi E, Salehi-Pourmehr H, Hashim H. Efficacy of combination therapy of mid-urethral sling and low-dose Abobotulinumtoxin-A injection in mixed urinary incontinence. Neurourology and Urodynamics. 2022; 41: 211-219
Legends to Figures
With permission from Wiley and Sons (Order no. 5682820593673, December 5, 2023)