




Case 1:
A 46-year-old female patient presented with the complaint of mixed urinary incontinence (UI) who was referred to undergo a mid-urethral sling surgery. She was on oral diabetics for her type 2 diabetes and had two vaginal deliveries. On physical examination, she was found to have Grade I anterior + posterior vaginal wall prolapse, a mobile urethra, and a negative ICS cough stress test and also negative accessory stress tests. Her quality of life was significantly affected by her UI, but she couldn’t delineate any predominant type of UI. Her urine analysis and urinary ultrasound were normal, and she had no residual urine after voiding.
With these findings, she underwent a standard ICS urodynamic testing, including filling cystometry and a pressure flow study.
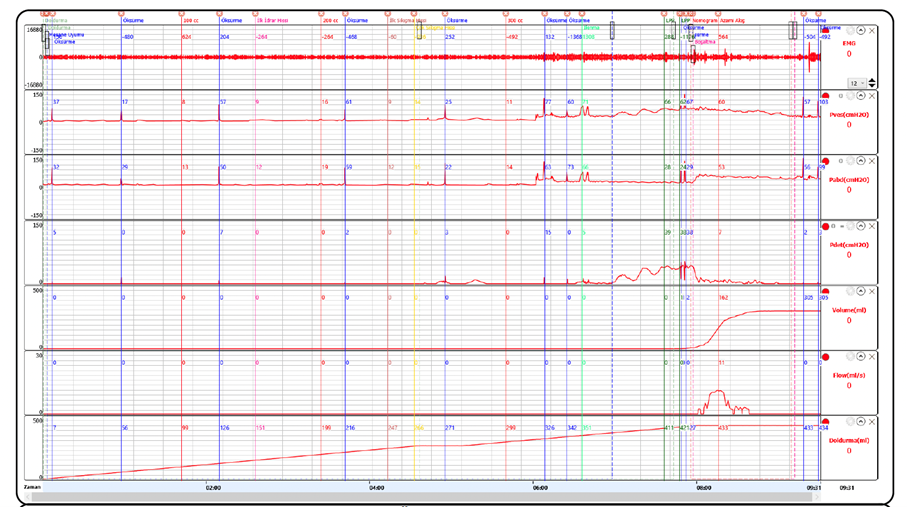
Her cystometry revealed normosensitive, normocompliant bladder with a normal capacity.
But with terminal detrusor overactivity and urinary incontinence. Her cough tests throughout the study again were negative. A standard pressure flow study could not be performed because she started to leak urine before the permission to void. But still, one could tell that her bladder outflow was not obstructed. The patient started antimuscarinic treatment; thereafter, her urgency component was completely resolved. She is happy now and occasionally experiences stress urinary incontinence, only with very strong coughs and only when the bladder is full, which does not affect her Q/L.
The management of mixed UI is challenging, and the predominant type is not always easy to understand. These cases need an invasive urodynamic study to objectively assess lower urinary tract dysfunction, besides a thorough clinical evaluation before irreversible therapies are applied.
Case 2: A 50-year-old lady presented with persistent stress incontinence with cough and exercise despite TO-MUS surgery one year ago.
She had five vaginal deliveries and no co-morbidity. On physical examination, she was found to have a urethra with limited mobility (Qtip tests <30 degrees) and a positive ICS cough stress test, no prolapse, and no mesh erosion. Her tape was palpated suburethral in the correct localization without any other abnormality. She had normal uroflowmetry with no residual urine. Her biochemical and ultrasound assessment was unrevealing.
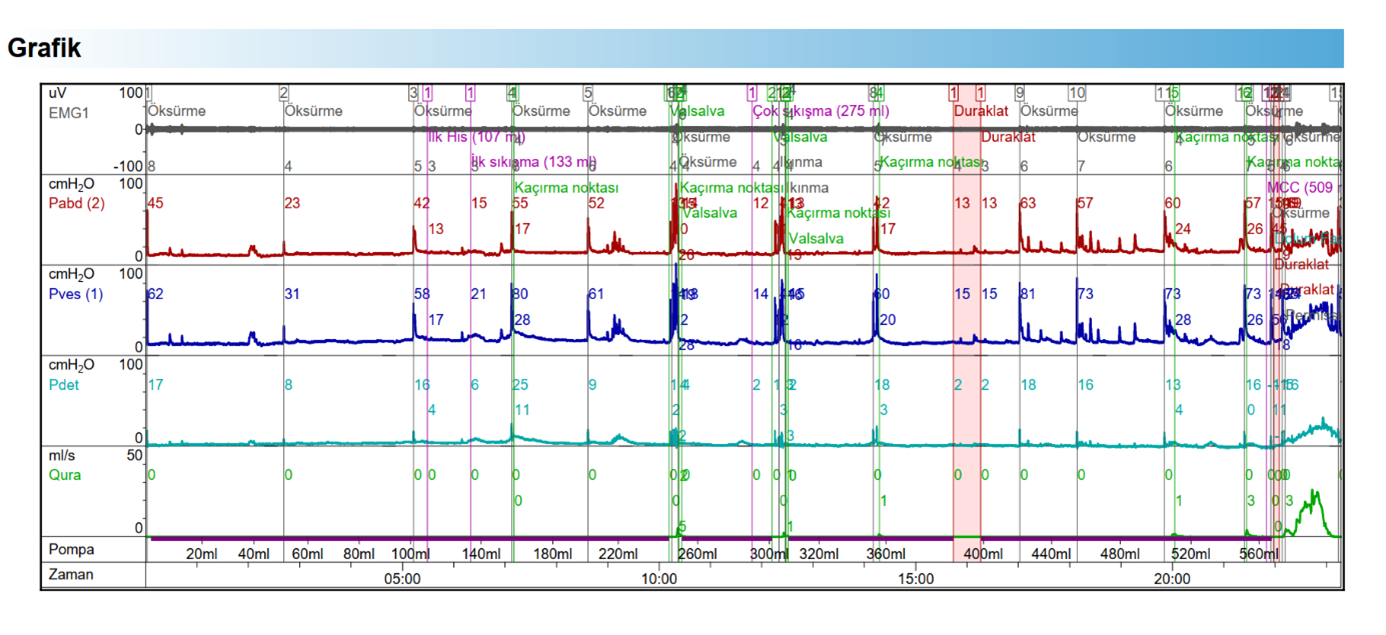
Her cystometry revealed normal bladder capacity and sensation, normal compliance, and no detrusor overactivity but urodynamic stress UI with low ALPP (<60 cmH2O), which was manifest with every cough test after 300 ml of bladder volume. Her pressure flow study was normal.
Considering her limited urethral mobility and low ALPP, she was offered to undergo autologous fascia pubovaginal sling surgery with vaginal partial mesh excision. Edward McGuire introduced intrinsic sphincter deficiency (ISD) as a distinct etiology of female SUI in the 1970s, which still includes many unanswered questions. ISD is the main reason for surgical failures. The classical triad of management options for ISD includes autologous fascia pubovaginal slings, artificial urinary sphincter implantation, and periurethral injection of bulking agents. Urodynamic parameters such as low urethral closure pressures, low abdominal leak point pressures, or both may define ISD, but the methodology is imprecise and variable. Still, the present case is a good example of ISD, as revealed by invasive urodynamic studies.